A Way to Repair a “Leaky” Blood-Brain Barrier is Tested, Potentially Relevant for Schizophrenia, Autism and Other Disorders
A Way to Repair a “Leaky” Blood-Brain Barrier is Tested, Potentially Relevant for Schizophrenia, Autism and Other Disorders
A team of researchers co-led by a three-time BBRF grantee has developed a way to potentially repair the integrity of the blood-brain barrier (BBB), the protective membrane that separates the brain from the bloodstream. Leaks and other problems in the BBB have been linked in past research with neurodevelopmental illnesses such as autism and schizophrenia as well as neurodegenerative conditions such as Parkinson’s and Alzheimer’s diseases.
The BBB is composed of specialized endothelial cells (ECs) that separate the bloodstream from brain tissue. The barrier they form regulates the passage of substances into and out of the brain, protecting it from harmful toxins and microbes, as well as proinflammatory immune cells, while allowing essential nutrients and signaling molecules to pass into the brain.
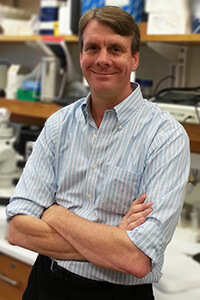
Investigators reporting new research in the journal Science Translational Medicine, led by BBRF grantee Stewart A. Anderson M.D., and Jorge Ivan Alvarez, Ph.D., both of the University of Pennsylvania, have previously found impairment in the BBB in mice that model the human genetic condition called 22q11.2 deletion syndrome (22qDS). 22qDS involves the deletion of roughly 45 genes on one copy of chromosome 22, and is associated with neurodevelopmental disorders including intellectual disability, autism, and ADHD.
Dr. Anderson, a BBRF Scientific Council member, 2016 BBRF Independent Investigator and 2002 and 1995 BBRF Young Investigator, and another team member, Adam J. Rossano, M.D., Ph.D., a 2023 BBRF Young Investigator, have both conducted grant projects focusing on the role of mitochondria—the ubiquitous energy “factories” that power our cells—in the context of pathologies thought to occur in schizophrenia and psychosis.
“Little is known about the role of the mitochondria in the BBB,” the team notes in their paper, although it has been demonstrated that ECs in the BBB have a much higher mitochondrial content than ECs elsewhere in the body (i.e., outside the brain). This suggested to the team that ECs in the BBB may be unusually dependent upon mitochondria.
The new study is driven in part by the prior finding of BBB impairment in mouse models of 22qDS, but also by the previously established fact that among the 45 genes deleted in 22qDS, at least 6 encode proteins that localize to mitochondria. The researchers set out to study whether mitochondrial deficits contribute to BBB dysfunction in 22qDS, and whether this, in turn, might be linked to behaviors seen in people and mouse models of 22qDS—specifically, social deficits.
The team used induced pluripotent stem cell (iPSC) technology in some of their experiments, which enables investigators to study, in cell cultures or following transplantation into animals, pathologies that occur in the human brain. Some of these pathologies are thought to underlie neurodevelopmental disorders such as autism spectrum disorders and schizophrenia. Blood or skin cells are sampled from affected patients and then reprogramed to become stem cells that can be redeveloped as specific cell types such as neurons. Importantly, the new cells retain the disease-linked genetic variations of the original donor.
In this study, the team generated endothelial-like cells from stem cells derived from 22qDS patients who also were diagnosed with schizophrenia, as well as from controls. The researchers then conducted experiments showing mitochondrial impairment, including a deficit in ATP production in these cells. ATP is the main energy transfer molecule in cells that powers cellular and organ functions throughout the brain and body. Mitochondrial impairments were also seen in BBB endothelial cells from mice genetically modeling 22qDS syndrome.
On the basis of these results, the team proposes that mitochondria are indeed dysfunctional in the BBB in 22qDS—and possibly in other disorders in which BBB integrity is impaired and a source of pathology.
A separate set of experiments in both the 22qDS model mice and in the stem cell-derived human BBB cells involved treatment with a drug called bezafibrate. FDA approved, it is used to treat hyperlipidemia (high blood lipid levels), by lowering "bad" cholesterol and raising "good" cholesterol. Treatment with drugs of this type—stimulators of activity at PPAR receptors, which help regulate, among other things, the generation and turnover of mitochondria, have generated positive results in animal-model experiments pertinent to stroke, epilepsy, schizophrenia, and Alzheimer’s.
In both in the stem cell-derived BBB and the 22qDS mouse model, bezafibrate improved mitochondrial generation of ATP, and improved measures of BBB “leakiness.” It is possible that functional BBB improvement is a direct consequence of the drug’s effect, but, the team noted, it is also possible that at least in the 22qDS mouse model, the drug’s impacts on LDL cholesterol, reducing triglycerides, improving glucose sensitivity, and decreasing blood glucose levels might also have had influenced BBB function. Further experiments could reveal mechanisms more specifically.
After drug treatment, the team also observed upregulation, i.e., increased expression, of mitochondrial genes in ECs from the BBB in the model mice, another bit of evidence suggesting the drug’s BBB-strengthening effects.
Importantly, treatment with bezafibrate also corrected deficits in social memory in the mice modeling 22qDS. This kind of deficit has been previously linked with BBB dysfunction. Again, it is possible, but not certain, that this outcome was influenced by bezafibrate directly affecting neuronal functioning, the team said.
Overall, the researchers suggest their experiments indicate that mitochondrial dysfunction in the BBB influences both BBB integrity and behaviors that may result from breaches, and “identify a potential therapeutic mechanism by which the BBB may be targeted in these conditions.”