Alterations in Inhibitory Control After Eating Are Seen in Women with History of Bulimia Nervosa
Alterations in Inhibitory Control After Eating Are Seen in Women with History of Bulimia Nervosa
Researchers investigating the brain mechanisms underlying bulimia nervosa have reported new results, which, if replicated, could have implications for the way this eating disorder is treated.
Bulimia nervosa is a common eating disorder, and one of the most common psychiatric conditions in women. Core symptoms include out-of-control overconsumption of food (“binge eating”), followed by “compensatory” behaviors such as self-induced vomiting. Between binge or binge/purge episodes, food intake is often rigidly restricted or can be avoided completely. It’s estimated that symptoms persist in 60% of those who receive first-line treatment; the illness is also associated with elevated mortality rates.
In healthy adults, research indicates that food intake is regulated by processes in the brain related to inhibitory control, as well as by signaling that indicates one’s “metabolic state,” i.e., whether one has recently eaten (and is full) or has fasted (and is hungry).
Researchers led by 2020 BBRF Young Investigator Laura A. Berner, Ph.D., of the Icahn School of Medicine at Mount Sinai, note that in their alternation between extremes of “overcontrolled intake” (e.g., dietary restriction or fasting) and “disinhibited intake” (e.g., binge eating), people with bulimia appear to have an aberration in brain mechanisms that normally allow people to flexibly exert cognitive control to optimally match their metabolic state.
In a paper in Molecular Psychiatry reporting the results of their new experiments, the team, which included three other current and past BBRF grantees, describes the recent development of computational models which frame inhibitory control as an adaptive process that requires moment-to-moment decision-making about whether to engage in or stop a given behavior, such as eating. This modeling takes into account how people use experience to update beliefs about how likely it is that they will need to inhibit their behavior in the next moment in time.
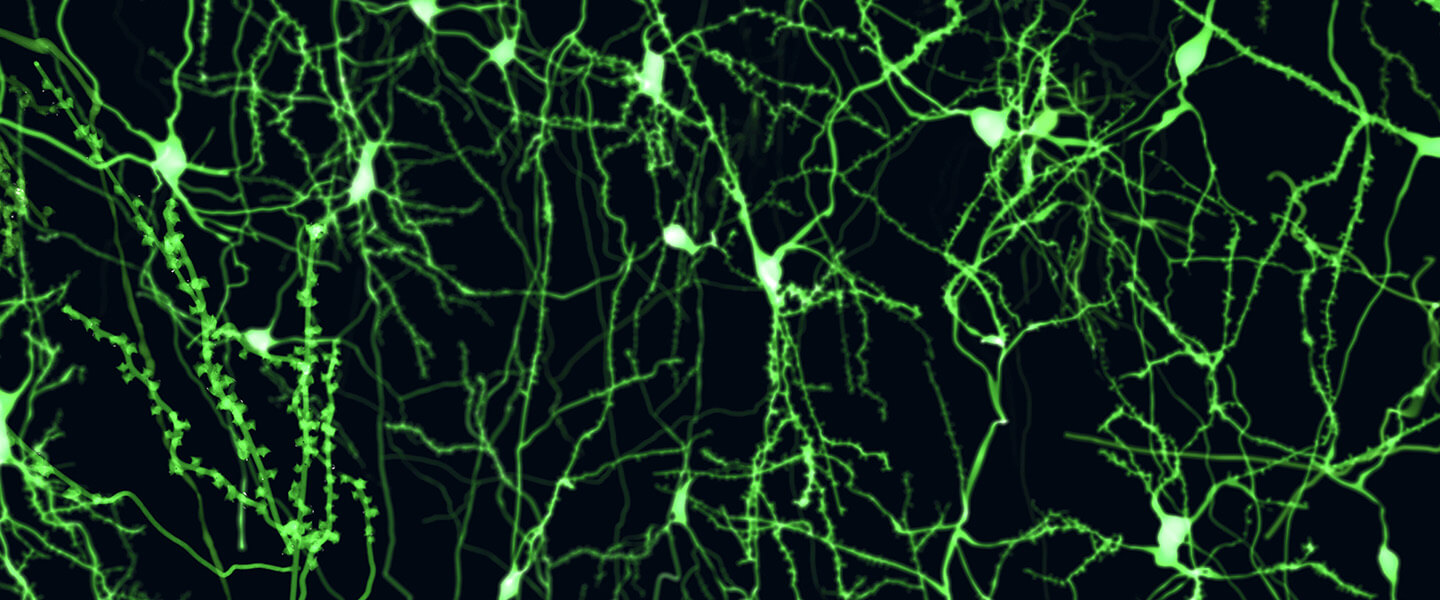
Such modeling has been integrated with functional MRI scanning of the brain to learn more about how inhibition and cognitive control work in both healthy people and in those with other disorders marked by behaviors that can feel out of control, such as substance use disorder. Dr. Berner and colleagues have now applied this integrated approach involving mathematical modeling of behavior and functional brain imaging to study bulimia nervosa.
They acquired data for 22 women who were in remission from bulimia and 20 matched controls with no psychiatric or metabolic disorders. All of these women performed a so-called “stop-signal task” (SST) testing cognitive control, while undergoing an fMRI scan—once, after a meal, and once after a 16-hour fasting period. “Remission” was defined as maintaining a body weight above 85% of ideal weight, having regular menstrual cycles, and abstinence from binge eating, purging, and restrictive eating for at least 1 year. Women in remission were recruited to avoid potentially confounding effects of electrolyte disturbances or recent extreme fluctuations in metabolic state that are present in women with current symptoms of bulimia nervosa.
The results suggested that in bulimia nervosa, eating and fasting may aberrantly influence a signal in the brain’s striatum for what researchers call “control-related surprises.” The striatum coordinates multiple aspects of cognition, including action planning, decision-making, motivation, reinforcement, and reward perception.
The “control-related surprises” seen in women who were in remission from bulimia nervosa involve a specific kind of “prediction error” that is ultimately related to the brain’s ability to know when to modify a current behavior. Called “unsigned prediction error,” this kind of processing error registers an individual’s surprise that they either need or don’t need to exert control.
Large prediction errors of this kind indicate that a person’s expectation about whether control is needed is inaccurate, and that behavior should be adjusted. The researchers found that after eating, unlike women without any eating disorder history, the women remitted from bulimia showed lower activation for “control-related surprises” in the left dorsal caudate region of the striatum. Through its connections with the prefrontal cortex, the dorsal caudate is thought to “play a central role in cognitive control by updating control-related predictions.” The lowered level of activation for unsigned prediction errors in this brain region is similar to what has been repeatedly observed in studies of people with substance-use disorders.
Translated into behaviors in bulimia nervosa, altered activation for these surprises might make it harder for a person to switch to a different behavioral strategy (e.g., stopping eating) when changes in internal or external states occur (e.g., when one has been eating and should feel full). In line with this idea, altered activation following eating was most pronounced (i.e., lowest) in women with histories of more frequent past binge eating and self-induced vomiting. Therefore, results suggest that alterations in inhibitory control processing in the brain, calibrated to whether one has recently eaten or not, may contribute to behaviors seen in patients with bulimia nervosa.
Because participants in the study with a history of bulimia were in remission at the time of the study, it was not possible for the team to determine if the altered signal that was detected is a trait of the illness, a scar of having had it, or a contributor to recovery. Dr. Berner and colleagues are now testing to see if this altered signal is present also in women with active symptoms of bulimia nervosa, and whether it drives and predicts changes in binge eating, purging, and the over-controlled eating often seen in the disorder.
As for implications in treatment of bulimia nervosa, the team noted that current behavioral treatments for the disorder focus first on eliminating periods of food restriction. But, they said, “if a blunted signal for control-related surprises makes inhibition more difficult after eating, then treatments that focus on the ‘fed’ state may prove fruitful.” They go on to say that interventions that can enhance cognitive control—non-invasive brain stimulation, or behavioral skills practice—may be most effective if delivered during or immediately after food consumption. The results also suggest a potential target (left dorsal caudate) for future interventions or development of biomarkers for disease severity, the team said.
The team also included: Martin P. Paulus, M.D., BBRF Scientific Council and 2000 BBRF Young Investigator; Alan N. Simmons, Ph.D., 2006 BBRF Young Investigator; and Katia M. Harlé, Ph.D., 2021 BBRF Young Investigator.



