Non-invasive Brain Stimulation Reduced Fear and Anxiety in a Preliminary Trial
Non-invasive Brain Stimulation Reduced Fear and Anxiety in a Preliminary Trial

Researchers have reported success in a preliminary effort to use non-invasive brain stimulation to reduce fear and anxiety. The placebo-controlled trial involved 19 healthy human subjects who were exposed to stimuli designed to activate their “startle” response to an experienced or anticipated threat.
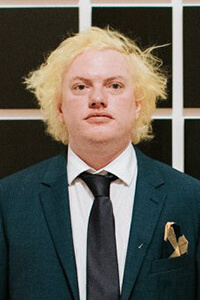
The experiments grew out of a project funded by a 2018 BBRF Young Investigator grant to Nicholas Balderston, Ph.D., now at the University of Pennsylvania. Dr. Balderston and colleagues used repetitive transcranial magnetic stimulation (rTMS) to reduce excitation in a part of the brain called the parietal lobe. Specifically, they targeted a section called the IPS (intraparietal sulcus), which their past research had shown to be “hyperexcited” when individuals are experiencing or perceiving a threat.
As Dr. Balderston’s team noted, in a paper published in the journal Translational Psychiatry, nearly one American in five meets the criteria for an anxiety disorder each year, and less than half of these individuals receive treatment that is even “minimally adequate.” While there are a number of pharmaceutical treatments for anxiety, as wells as various forms of talk therapy, the researchers said they wanted to “broaden the scope” of potential treatments by learning more about the potential of non-invasive brain stimulation to help patients.
rTMS has been FDA-approved for depression since 2008, and has an effectiveness profile that often compliments that of antidepressant medicines, which don’t help every patient achieve remission. But rTMS has not been as successfully or broadly applied in anxiety disorders. Dr. Balderston’s team wanted to test rTMS in a mode called “low-frequency,” which reduces excitation in targeted brain areas—in this case, the IPS. (“High-frequency” rTMS, which increases cortical excitation, is used in treating depression.)
The team enrolled 19 subjects in a double-blinded trial of rTMS under a variety of test conditions. The subjects were healthy and averaged about 30 years of age; 13 were female. Participants were exposed to threats: brief, mild electric shocks to the wrist which were uncomfortable but harmless. These challenges were delivered in separate “runs”: in some they were predictable and in others unpredictable. Fear and anxiety caused by the anticipation of predictable and unpredictable threats was measured by quantifying participants’ startle response.
While these challenges were being presented, in successive rounds, all of the participants experienced them, in turn, while receiving low-frequency rTMS targeting the IPS; a simulated (placebo) version of rTMS that did not actually deliver stimulation to the brain; and a “no-rTMS” mode where the equipment was not even present.
The team found that when rTMS was being directed to the IPS, there was a measurable reduction in the “startle” response caused by both fear and anxiety, compared with the startle response with placebo rTMS and no-rTMS.
The researchers think these results indicate that the parietal cortex plays a causal role in a state of elevated arousal that regulates the startle response. Further, they suggest that using rTMS to reduce excitability in the IPS can “reduce physiological arousal associated with fear and anxiety during threat.”
Although additional research should help to clarify these ideas, the team believes that by inhibiting activity in the parietal cortex while a threat was being experienced, “it’s possible that we were reducing subjects’ tendency to shift their attention towards the shock threat,” and in this way reducing their threat-related anxiety. This is interesting in part because the IPS region of the parietal lobe is known to be involved in focusing attention, among other things.
Based on its findings, the team thinks low-frequency rTMS is a potential treatment for anxiety disorders, a prospect they intend to explore in larger trials involving patients diagnosed with generalized anxiety disorder—trials that must also test what proportion of patients are helped, to what degree, and for how long.
Other members of the research team, in addition to Dr. Balderston, included senior member Christian Grillon, Ph.D., a 1988 BBRF Young Investigator; Sarah Lisanby, M.D., a 2010 BBRF Distinguished Investigator and 2003 Independent Investigator; and Zhi-De Deng, Ph.D., a 2017 BBRF Young Investigator.