Early Diagnosis and Intervention Techniques for Children
Early Diagnosis and Intervention Techniques for Children
From The Quarterly, Spring 2013
Attention-deficit hyperactivity disorder (ADHD) is the most commonly diagnosed
neurobehavioral disorder in children, but its diagnosis has been controversial.
Without specific biological markers, diagnosing mental illness in children is difficult. ADHD diagnosis has traditionally depended on the presence of particular behavioral traits, mainly hyperactivity, impulsivity and inattention, but these traits can differ at different ages and can be different in boys and girls.
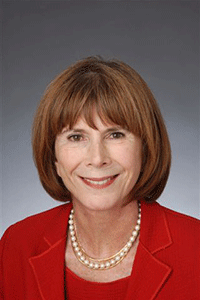
Dr. Klein, a founding member of the Brain & Behavior Research Foundation
Scientific Council, is a leader in research on childhood mental health. Her long-term studies have helped to confirm ADHD as a true brain disorder, and point to the need for tailored approaches to prevent and effectively treat disorders in children.
How can actual brain disease be sorted out from normal variations in children’s behavior? ADHD usually has a family history. A strong genetic component has been demonstrated in landmark twin studies; twins raised by adoptive parents have a considerably higher than average percentage of ADHD if a biological parent had the disorder.
The advent of powerful methods of brain imaging has revealed alterations in the brains of patients with ADHD. Dr. Klein and colleagues recently completed an imaging study of people now 41 years old who had been diagnosed with ADHD at age eight. Compared to controls followed for the same period of years, all of them showed smaller brain volumes whether or not they were still diagnosed with ADHD.
ADHD is currently treated with either stimulant drugs or behavioral therapy, or a combination of the two. Amphetamines and methylphenidate (Ritalin), have been in use for many years, but they were not systematically evaluated until the 1960s and 1970s. Previously, their main disadvantage was that they were short-acting. Long-acting, oral and patch-delivery forms are now available, and are effective for the majority of ADHD patients. By contrast, behavior therapy for ADHD, introduced in the 1960s, has not been shown to be as effective as medication and involves intensive application and considerable cost. A collaborative study in which Dr. Klein participated showed that outcomes for patients treated with medication combined with two years of intensive psychosocial therapy worked no better than medication alone.
With regard to concern about potential dangers of long-term use of stimulant medications, Dr. Klein’s follow-up studies of children taking these medications for periods of up to five years has yielded no evidence of negative effects.
Rachel G. Klein, Ph.D.
Fascitelli Family Professor of Child and Adolescent Psychiatry,
New York University Child Study Center;
1995 NARSAD Distinguished Investigator Grantee,
2004 Brain & Behavior Research Foundation Ruane Prize for Outstanding Achievement in Childhood and Adolescent Psychiatric Research,
Scientific Council Member
Women’s Mental Health Conference:
The Art & Science of Caring
On September 14, 2012 in New York City, the Brain & Behavior Research Foundation hosted the Women’s Mental Health Conference: The Art & Science of Caring. The event included a panel discussion on Early Intervention, Rehabilitation and Reintegration; small group discussions with leading researchers across mental illnesses; and a final panel discussion on overcoming stigma and the future of public policy and research. This is a highlight of some of the presentations. Full transcripts of the talks are available at bbrfoundation.org/2012-WMHC.