Moving Beyond ‘Chemical Imbalance’ Theory of Depression
Moving Beyond ‘Chemical Imbalance’ Theory of Depression

A ‘bottom up’ approach to understanding the brain leads to crucial new discoveries
From The Quarterly, Fall 2012
What causes depression? Experience tells us that people can become depressed when they are under acute or chronic stress. Or when they are exposed to trauma. It tells us that the period immediately following childbirth often finds new moms in a ‘blue’ mood. We also know that some people who lose a loved one stay ‘down’ even after an extended period of grieving.
But all of these are associations between certain life experiences and depression, not biological causes.
And they tell us nothing about why millions of other people, for no apparent reason at all, experience plunges in mood that leave them incapable of experiencing pleasure, even in rewarding activities and experiences that almost universally produce it.
The first attempts at defining depression as a biologically-based illness hinged on a theory of ‘a chemical imbalance in the brain.’ It was thought that too much or too little of essential signal-transmitting chemicals—neurotransmitters—were present in the brain. Treatments were developed to keep neurotransmitters (such as serotonin) within the tiny gaps called synapses between adjacent nerve cells, where signals are exchanged. By preventing specific neurotransmitters from being reabsorbed into nerve cells, the theory went, the signals between cells would be boosted and mood would be lifted. The most popular antidepressant medications, such as Paxil® and Prozac®, were developed to function in this manner. Unfortunately, the alleviation of depression’s symptoms with these treatments remains elusive; they are ineffective for as many as 50% of patients with depression.
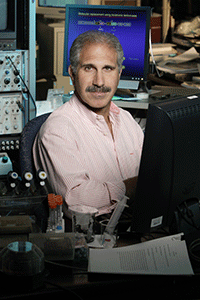
“This idea of chemical imbalance has been useful—that you have a kind of chemical soup in which there may be too much dopamine or too little serotonin,” says Robert C. Malenka, M.D., Ph.D., a Brain & Behavior Research Foundation Scientific Council Member, three-time Foundation Grantee, and the Pritzker Professor of Psychiatry and Behavioral Sciences at Stanford University School of Medicine.
“But in truth,” Dr. Malenka continues, “the ‘brain soup’ idea is no longer adequate.” It really has reached a dead-end. This is why antidepressants aren’t working for so many people—all the current medications work via these same mechanisms. Therefore, Dr. Malenka reasons, “there’s a great need to understand in greater detail the brain biology that underlies depression’s symptoms” so that novel therapies can be found.
Wanting to understand pleasure leads to a surprising discovery
Earlier this year, Dr. Malenka led a team of researchers conducting a series of experiments involving neurons in a part of the brain known since the 1950s to be associated with the ability to feel pleasure. This area, called the nucleus accumbens, or NAc for short, is part of what is often called ‘the pleasure circuit.’ He and his colleagues were exploring the idea that some malfunction in the NAc has an important connection with clinical depression’s most universal symptom: the inability to feel pleasure, which psychiatrists call anhedonia.
The NAc “has evolved over eons to promote our survival. It is activated during sex; during the pleasurable aspects of feeding. It’s the one that tells you warmth is really good when you’re cold; that water is great when you’re thirsty; that sleep is wonderful when you’re tired,” says Dr. Malenka. It’s the part, when functioning properly that tells us: ‘I should engage in behaviors that increase my chances of experiencing this rewarding event again.’” If this all-important circuit isn’t working properly, anhedonia is the result.
The research team made an unexpected discovery. They found that a hormone known to affect appetite, called melanocortin, turns off the brain’s ability to experience pleasure when an animal is stressed. And it was happening, importantly, in the NAc part of the brain. “A few scattered studies had suggested that chronic stress increased melanocortin levels in the brain, but it wasn’t yet known, whether melanocortin actually affected the nucleus accumbens or how,” said Dr. Malenka. This is the first study to implicate melanocortin in depression. These new findings could lead to an entirely new class of antidepressant medications.
Recognizing the brain as a vast network
Dr. Malenka notes that research performed by others makes strong connections between problems in the NAc and conditions as diverse as addiction, obsessive-compulsive disorder (OCD) and schizophrenia. This curious fact gets at the central problem that has motivated Dr. Malenka’s highly successful 30-year career in neuroscience.
“It turns out that everything in the brain is more complicated than we might imagine. Everything we study involves interactions between different brain areas and therefore different circuits and different modulators of those circuits.”
In moving beyond the comparatively simple ‘chemical imbalance’ model, Dr. Malenka and others don’t mean to imply that neurotransmitters like serotonin or dopamine are unimportant. The problem is that both of these neurotransmitters, and others, “influence circuit activity in many complex ways in many different brain areas and many different circuits. And it’s not as if every one of those circuits is dysfunctional in, for example, depression.”
Dr. Malenka is a leading expert on those tiny gaps called synapses across which nerve cells transmit signals. There are trillions of synapses in the human brain. The grand challenge of Dr. Malenka’s career has been to understand how these critical signal-junctions operate, and to relate this fine-grained knowledge to what goes wrong in specific circuits to cause the symptoms of illnesses such as depression or OCD or addiction. For his work, he received the Brain & Behavior Research Foundation 2010 Goldman-Rakic Prize for Outstanding Achievement in Cognitive Neuroscience.
Of the support from the Foundation he has received, Dr. Malenka said, “Having been supported with a NARSAD Young Investigator Grant and later with a NARSAD Distinguished Investigator Grant, the Foundation has provided me with valuable financial support to pursue ideas that were ‘outside the box.’ But it also has given me the acknowledgment that the research ideas were worth pursuing.”
“In one part of my work, I’ve studied very basic mechanisms involving, for instance, the molecules involved in synaptic transmission and changes of synaptic strength,” which are associated with learning and memory. Many of these molecules he studies—proteins called neuroligands and neurexins—when they are abnormal have been found to contribute to pathology in disorders like autism and schizophrenia. Many of the genetic studies the public hears about, in which gene mutations are associated with one or another psychiatric illness, often identify defects in genes that instruct cells to manufacture these vital proteins Dr. Malenka has studied at the synapse.
“We can’t study every genetic variant, or every brain region, and certainly not every synapse,” Dr. Malenka reasons. “It’s just impossible. So we have to make educated guesses based on our knowledge that variation in many different genes predisposes to similar disorders.”
This is a hopeful observation. It leads Dr. Malenka and others to proceed on the hypothesis that pathways and circuits, numerous though they may be, seem to converge on disturbances in a finite set of essential brain functions.
Targeting malfunctioning circuits may treat symptoms across disorders
His team’s discoveries about the melanocortin circuit’s contribution to anhedonia-like behavior identify a potential new pathway of intervention in depression, beyond adjusting neurotransmitter levels. It focuses specifically on identifying and correcting the melatonin circuit malfunction that stress appears to cause, which in mice was linked with the inability to engage in pleasurable activity.
There is the prospect that detailed circuit-knowledge of this kind may lead to an entirely new way of treating disorders as different as depression and schizophrenia.
One might, for example, treat anhedonia, or the inability to be motivated by the prospect of reward, whether this symptom occurs in a person diagnosed with major depression or some other illness. Indeed, many people with schizophrenia are observed clinically to be unable to motivate themselves, or when motivated, find it very hard to convert that thought into action. A future medication that acted on melanocortin receptors to address anhedonia might help such a patient, who would continue to take other medications to control other symptoms seen in schizophrenia but not depression, such as psychosis.
The idea to look at diseases through the lens of malfunctioning circuits and relays in the brain and the symptoms they cause is being explored in Foundation-funded NARSAD Grants to many scientists like Dr. Malenka. This path of research promises to bear a harvest of great value in the years ahead.