Functional Connectivity Brain Changes Involving Linkages Between Cognition and Motor Function Are Discerned in OCD Patients
Functional Connectivity Brain Changes Involving Linkages Between Cognition and Motor Function Are Discerned in OCD Patients
The symptoms of obsessive-compulsive disorder (OCD) can be debilitating. Those affected experience intrusive, distressing, and often irrational thoughts (“obsessions”) which are accompanied by repetitive physical or mental acts (“compulsions”). OCD is quite common, thought to occur in 1% to 3% of the global population. It affects both young people and adults, and takes a vast variety of forms.
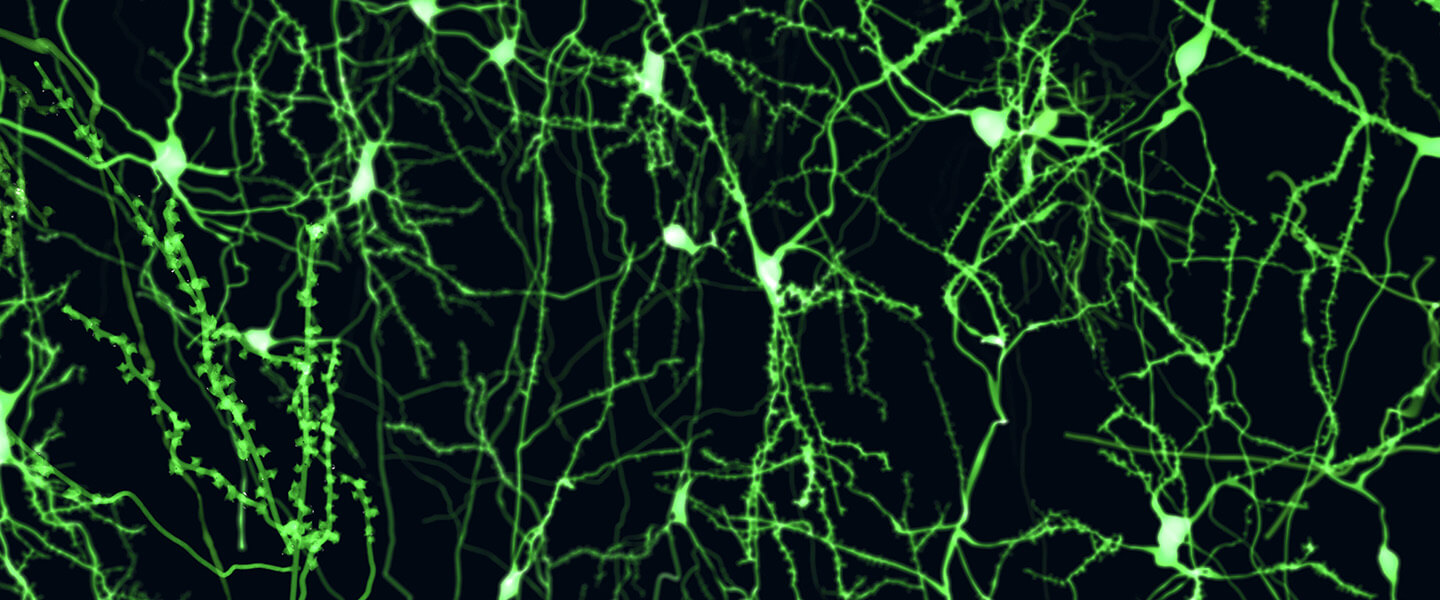
Efforts have been made to determine the biological underpinnings of OCD symptoms, based largely on functional brain scans in which those with the diagnosis are compared with those who are unaffected. These studies have directed the attention of the research community to a set of brain circuits referred to with the acronym CSTC (cortico-striato-thalamo-cortical). These circuits running between the brain’s cortex, striatum, and thalamus, are complex and involve feedback loops, i.e., flow between regions that are not uni-directional but which “feed back” to affect one another on an ongoing basis. In broad terms, the CSTC circuitry is involved in a wide array of brain processes: cognition, affect, motivation, and motor functions.
Recent research has also suggested involvement in CSTC circuitry of the brain’s sensorimotor circuits, which are involved in the generation and control of motor behaviors and the integration of information from the senses. This circuitry seems “particularly relevant to OCD” given its role in habit formation and mechanisms that normally serve to inhibit non-essential, unwanted, or irrelevant information, notes a large international research team in a new paper appearing in Molecular Psychiatry. Dysfunction in this circuitry, they note, “could be related to the inability of OCD patients to suppress internally triggered repetitive and intrusive thoughts and behavior.”
The team, composed of over 100 investigators, many affiliated with a consortium called ENIGMA-OCD (Enhancing Neuro-Imaging and Genetics through Meta-Analysis), report on their most recent effort to probe functional connectivity in OCD patients, in part to discern how connectivity in those with OCD differs from that in healthy controls, and in part to test for biomarkers which might enable clinicians to distinguish people with OCD from those not affected.
The team’s four senior members included Odile A. van den Heuvel, M.D., Ph.D., 2009 BBRF Young Investigator; Paul M. Thompson, Ph.D., 2017 BBRF Distinguished Investigator; Dan J. Stein, Ph.D., FRCPC, 1991 BBRF Young Investigator; and corresponding author Guido A. van Wingen, Ph.D., of the University of Amsterdam, the Netherlands. Willem B. Bruin, Ph.D., was the paper’s first author.
Rather than focus on pre-determined regions of interest in the brain associated with circuitry already believed to be affected in OCD, the team investigated functional connectivity differences across the entire brain, using MRI data of 1,024 OCD patients and 1,028 healthy controls. Whole brain functional connectivity was assessed at both the regional and network (i.e., spanning regions) levels. The participants were scanned in 28 separate and independent samples within the overall ENIGMA project. The method used by the team is called “mega-analysis,” which involved pooling individual data across the 28 studies. This contrasts with the oft-used “meta-analytic” approach which synthesizes summary statistics from multiple studies to estimate an overall effect.
Most broadly, the mega-analysis revealed “widespread functional connectivity aberrations in OCD patients.” The most pronounced overall change relative to healthy controls was what the team calls “global hypo-connectivity,” with a few instances of hyper-connections. Hypo connections are circuits that show less connectivity than average; hyper connections show greater connectivity than typical.
Most notable among the differences in OCD patients was “significant hypo-connections located within the sensorimotor network,” something that had not been stressed in prior research, moving the team to suggest that on the basis of their analysis (if validated) “neural models of OCD should be revised” to incorporate this feature.
Although there had been some evidence of its involvement in past studies, “the sensorimotor network is often overlooked in OCD studies,” the team notes, and it is not typically included in functional connectivity scans that focus on particular circuits or networks postulated in advance to be involved in OCD. Altered connectivity in OCD patients could reflect impairments in the process (called sensorimotor gating) of suppressing irrelevant sensory, cognitive, and motor information, which may contribute to the inability of OCD patients to inhibit undesired thoughts and images and repetitive behaviors or thoughts.
The team found no aberrations in OCD subjects in what is generally considered the most important part of the CSTC, the frontostriatal loop (pathways that connect the frontal lobe with the basal ganglia, which mediates motor, cognitive, and behavioral functions).
Regarding another of their objectives, the team reported that despite observations of global hypo-connectivity in patients at the group level, their application of machine learning to the results showed that functional connectivity cannot at this time provide an accurate distinction between patients and controls. In other words, the signal is not sufficient, on its own, to serve as a reliable and highly accurate biomarker that clinical use would demand.
The team suggests that the difficulty in applying the widely observed “hypo-connectivity” signal to diagnosis has to do with OCD’s heterogeneity—the considerable variance among different individuals with the disorder, in terms of, for instance, sex, age of onset, severity, medication status, and perhaps most of all, symptoms. “Particular OCD subtypes may be characterized by different neural irregularities and functional changes,” the team said. Machine learning may eventually be able to make headway in defining biomarkers, but only after further studies that incorporate more detailed clinical information about participants and well as observation at different points in life and over the course of years. It is also possible that no biomarker applicable to the total set of OCD patients may be possible to establish, directly reflecting fundamental diversity within the group.
Other BBRF grantees on the team included: Alan Anticevic, Ph.D., 2015 BBRF Klerman Prize winner, 2015 BBRF Independent Investigator and 2012 Young Investigator; Chiang-Shan R. Li, M.D., Ph.D., 2009 BBRF Young Investigator; Erika L. Nurmi, M.D., Ph.D., 2008, 2010 BBRF Young Investigator; Christopher Pittenger, M.D., Ph.D., 2015 BBRF Independent Investigator, 2009, 2007 Young Investigator; Blair H. Simpson, M.D., Ph.D., 2010 BBRF Independent Investigator; Emil R. Stern, Ph.D., 2008 BBRF Young Investigator; Philip R. Szeszko, Ph.D., 2009 BBRF Independent Investigator, 2003, 1998 Young Investigator; Hein J. F. van Marle, M.D., Ph.D., 2022, 2018 BBRF Young Investigator.





