A Way of Predicting if New Psychosis Patients Will or Won’t Respond to Standard Treatment
A Way of Predicting if New Psychosis Patients Will or Won’t Respond to Standard Treatment
“Trial and error” remains the basis for care of people who have recently been diagnosed with psychosis, and “poor outcomes are common,” say a team of researchers at the University of California, Davis, led by BBRF Scientific Council member Cameron Carter, M.D. These facts have motivated the team to find a reliable, inexpensive, and easy-to-administer way of predicting who among recently diagnosed patients will and will not respond to existing treatments.
Being able to predict treatment response would be especially valuable for patients unlikely to respond to standard treatment; such patients might get an alternative treatment that’s more likely to help from the very beginning.
In a recently published article in the American Journal of Psychiatry the team reports that they have tested a method that was able to “significantly predict” which patients would and would not show an improvement of 20% or more in psychosis symptoms after one year of treatment. The 20% figure is a minimum threshold for improvement established by a large working group of experts on schizophrenia and psychosis in 2016 in an effort to make different clinical trials more readily comparable.
The treatment given to psychosis patients involved in the trial consisted of a low-dose atypical antipsychotic medicine accompanied by comprehensive care which included cognitive behavioral therapy [CBT], education and employment support, psychosocial education, and/or family support.
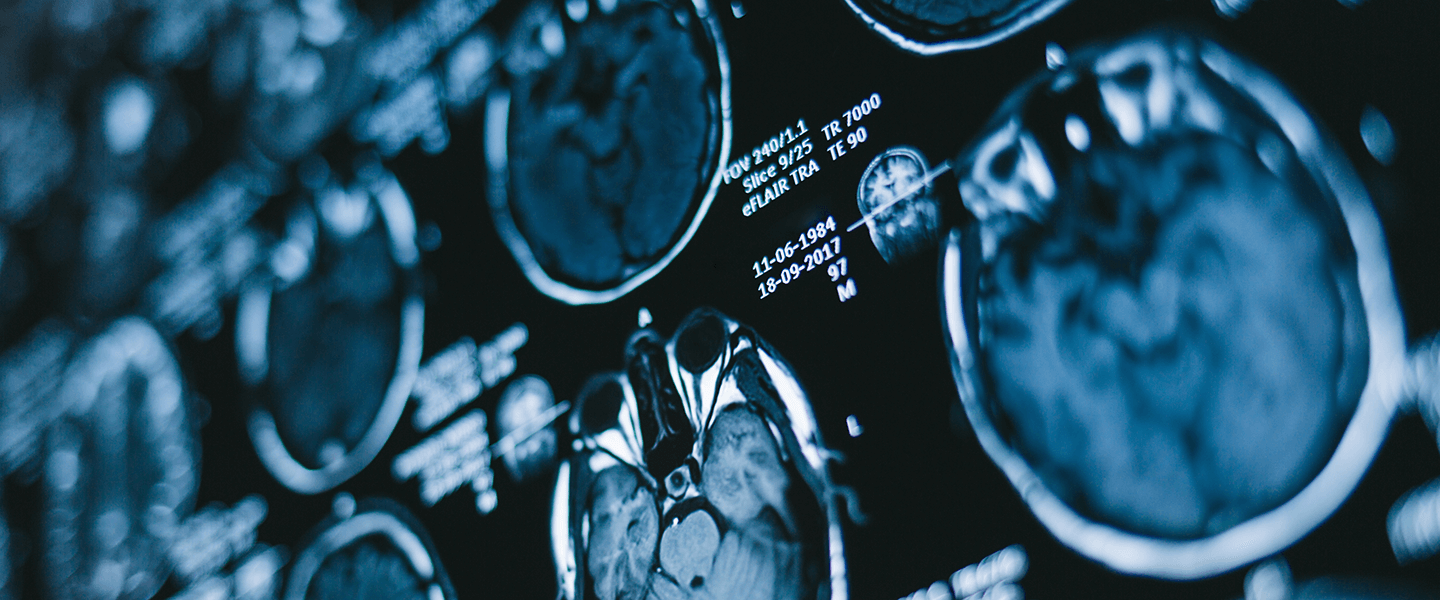
The predictive method used by Dr. Carter (a 2007 BBRF Distinguished Investigator, 1997 and 1994 Young Investigator and 2001 Klerman Prizewinner) and his colleagues, including Jason Smucny, Ph.D., first author of the paper, centers on analysis of fMRI brain scans made of each patient.
The 84 patients who took part in the trial received a scan within 2 years of their initial report of psychosis (65 had a diagnosis of schizophrenia and 17 of bipolar disorder). Scans were also made in 138 healthy control subjects for comparative purposes.
The point of the scans was to measure the level of activity in a specific part of the brain—the frontoparietal region—that is activated when an individual is exerting cognitive control. Cognitive control involves allowing information processing and behavior to vary from moment to moment rather than remaining rigid and inflexible. Activation of the frontoparietal region has been shown to be impaired in early psychosis.
Participants were asked to perform a cognitive task involving pressing buttons while they were undergoing their fMRI scan. Results showed that psychosis patients with greater activation in the frontoparietal region during this task were more likely to show symptomatic improvement at their 1-year follow-up. Just as important, the test also showed that poor activation in the same brain circuitry corresponded with poor response to treatment.
Discovery of this fMRI brain signal raises the question of which treatments are most effective in increasing activation in the frontoparietal region.
The antipsychotic medicine clozapine has been shown to have the desired effect, but it is usually prescribed only for patients who are not helped by other medicines, due to its potentially dangerous side effects and need for constant monitoring. Other forms of treatment could be tested in the future for their impact on the signal.
Although they say they have “taken a preliminary step” toward a method that can help patients, the team acknowledges that their fMRI signal is not ready for the clinic. The rate of successful prediction in the trial—70% for “improvers” and 60% for “non-improvers”—needs to be closer to 80% to justify widespread clinical use, the team said. They call for their method to be tested in larger groups of patients and combined with other kinds of predictive signals to achieve greater accuracy.
The importance of the study, the team suggested, was in demonstrating the frontoparietal fMRI signal as an objective biomarker, implicating that region mechanistically in psychosis pathology and relating it to symptoms in psychosis patients. It will also be important, the team says, to validate biomarkers that predict treatment response in terms of patients’ ability to function socially and occupationally, key objectives in recovery.



