Study: Ketamine Restores Neural Connection Points Lost in Stress & Depression
Study: Ketamine Restores Neural Connection Points Lost in Stress & Depression
Researchers led by 2013 BBRF Young Investigator Conor Liston, M.D., Ph.D., have just reported a surprising finding about the drug ketamine, concerning the way it acts on the brain.
Approved many years ago as an anesthetic, ketamine has been used in recent years—experimentally—as a rapidly acting antidepressant. Severely depressed patients have reported a dramatic lifting of symptoms within hours.
A “cousin” of ketamine called esketamine was approved by the F.D.A. in March 2019 for use in patients who have not been helped by two or more courses of conventional antidepressant treatment. But the new drug’s mechanism of action remains poorly understood. Many neuroscientists think it acts on the glutamate neurotransmitter system. Neurons sensitive to glutamate, an “excitatory” neurotransmitter, are by far the most common nerve-cell type in the human brain.
Dr. Liston and colleagues at the Weill Cornell School of Medicine in New York, with critical technical help from a team in Japan, wanted to take advantage of the fact that ketamine works rapidly to reduce depression-like symptoms in rodents as well as people. By administering the drug to rodents, they hoped to solve the puzzle of the drug’s action via sophisticated brain imaging techniques that reveal detail to the level of individual neurons and the microcircuits they form.
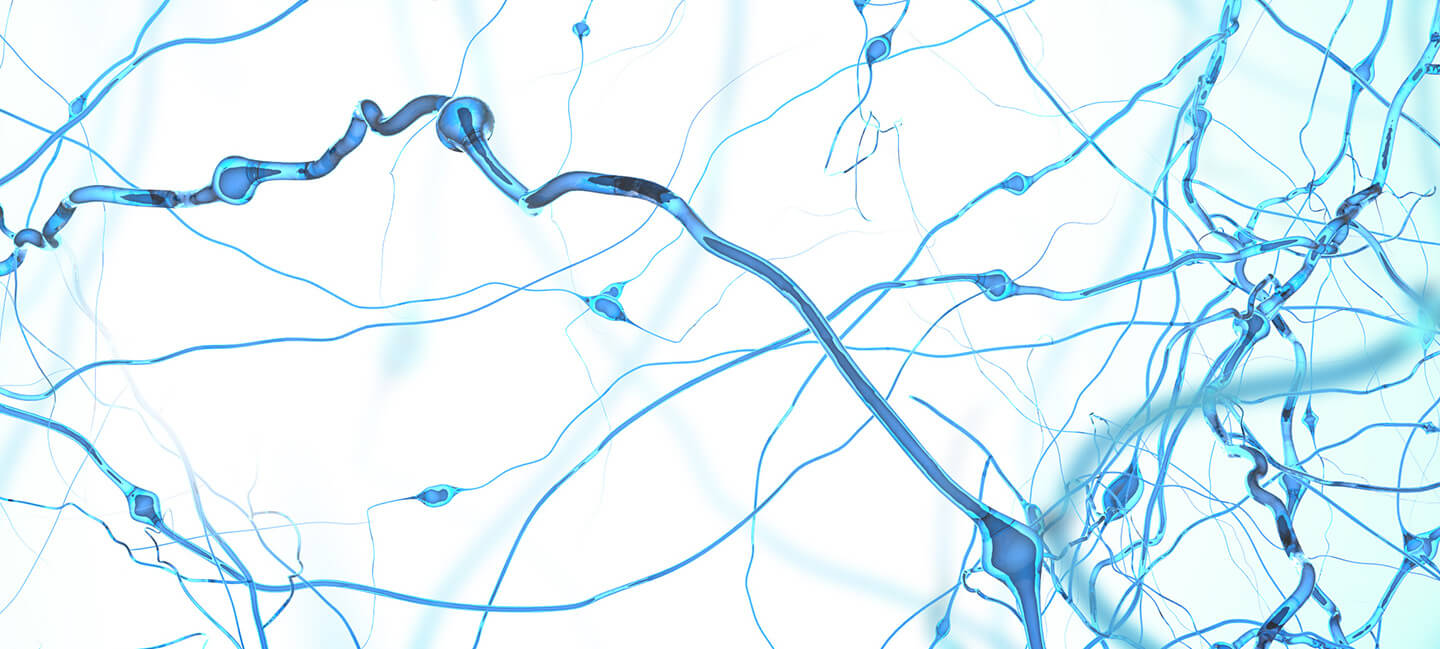
As they reported in the journal Science, the researchers noticed that an infusion of ketamine promotes the growth of tiny knob-like structures called dendritic spines. These provide connection points at synapses, tiny gaps across which neighboring neurons exchange information.
In depression, including depression caused by stress, dendritic spines of neurons in the prefrontal cortex tend to disappear. This is associated with reduced connectivity between neurons. Dr. Liston and colleagues intentionally caused spine loss in rodents by exposing them to physical stress and to stress hormone. Some of the same spines that disappeared were then observed to reappear following ketamine treatment; some new spines were also seen. Ketamine also restored activity among small groups of cortical neurons, forming microcircuits that are known to be involved in antidepressant behavior.
Surprisingly, however, the resurgence of spines did not occur until after ketamine’s behavioral impacts had already taken hold in the rodents. The initial antidepressant effect was therefore not attributable to the reappearance of lost spines. But further experiments demonstrated that unless new and restored spines were present, ketamine’s initial antidepressant effect could not be sustained.
While the new research leaves open the question of ketamine’s rapid onset of action, it does seem to account for how it sustains its impact—usually for about a week in human subjects. The new discovery suggests that therapies might be devised, such as pharmaceuticals or neural stimulation methods, that would aim to preserve or perhaps enhance the “rescue” of lost synapses, in order to sustain the benefits of ketamine and perhaps other rapid-acting antidepressants that are in development.