Researchers Discover a Role for Immune Cells Called Microglia in Inhibiting Brain Activity and Regulating Behavior
Researchers Discover a Role for Immune Cells Called Microglia in Inhibiting Brain Activity and Regulating Behavior
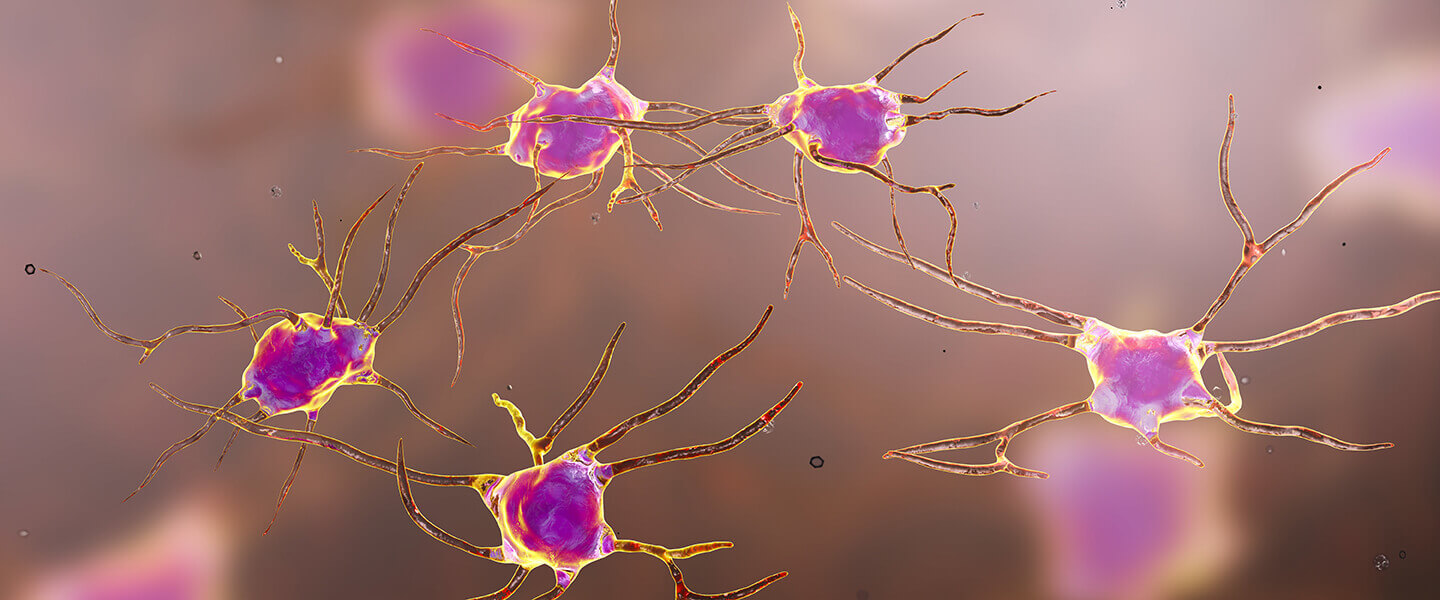
Researchers have discovered an entirely new way in which the healthy brain keeps neural activation within normal bounds. The finding, which uncovers an unexpected role of immune cells called microglia, has implications for our understanding of behavior as well as a number of illnesses that affect the brain.
For many decades, scientists have understood that brain activity, in broad terms, is the net result of forces that excite and inhibit neurotransmission. Excitatory neurons account for the bulk of activity, but a comparatively small number of inhibitory neurons strategically situated throughout the brain perform the essential role of tamping down excitation when it reaches critical levels.
This prevents neural circuits from becoming overexcited—a condition that can lead to brain seizures like those seen in epilepsy. Overexcitation also may be a factor in some psychiatric illnesses. A failure of the fetal brain to develop proper inhibitory circuitry is hypothesized to have a role in causing or raising risk for schizophrenia, autism, and possibly other disorders.
A team led by Anne Schaefer, M.D., Ph.D., of the Icahn School of Medicine at Mount Sinai, now reports in the journal Nature that cells called microglia—plentiful immune cells in the brain and spinal cord whose main functions include removal of dying neurons and pruning of unneeded synapses—also have a role in neural inhibition. They play this role, the researchers say, in the healthy brain, but this function is lost when their number is depleted and/or when inflammation is present in the brain or body, such as in neurodegenerative illnesses including Alzheimer’s and Parkinson’s diseases.
Dr. Schaefer was a 2010 BBRF Young Investigator. The team also included Paul Kenny, Ph.D., a 2015 BBRF Distinguished Investigator and 2004 Young Investigator; Erin Calipari, Ph.D., a 2018 BBRF Young Investigator; Dr. James Surmeier, Ph.D., a 1996 BBRF Distinguished Investigator; Munir Gunes Kutlu, Ph.D., a 2019 BBRF Young Investigator; and Pinar Ayata, Ph.D., a 2016 BBRF Young Investigator.
“When we think about brain function,” Dr. Schaefer says, “we typically think about how neurons control our thoughts and behavior. But the brain also contains large amounts of non-neuronal cells, including microglia, and our study puts a fresh spotlight on these cells as partners of neurons in the regulation of neuronal activity and behavior.”
The team’s experiments in mice revealed that microglia can sense neural activation by detecting a molecule called ATP that is released into extracellular space by active neurons and neighboring support cells called astrocytes. When microglia sense ATP, they physically extend tiny protrusions out into the environment toward the activated neuron, and trigger a cascade of chemical reactions that result in the local suppression of neural activity.
Dr. Schaefer explains that when inflammation is present, or in neurodegenerative diseases like Alzheimer’s, microglia lose their ability to sense ATP and thus their ability to regulate neural activity—perhaps a factor in the pathology associated with these conditions.
Since dysregulated neuronal activity is part of the pathology of an illness like Alzheimer’s, it means the regulatory role played by microglia also has an impact, indirectly, on behavior. This could also apply in the case of depression, which is hypothesized to involve inflammation in at least a subset of patients. In general, says Dr. Schaefer, “behavioral changes associated with certain diseases may be mediated, in part, by changes in communication between microglia and neurons.”
In future studies Dr. Schaefer and colleagues will explore the possibility that the ability of microglia to sense ATP may mean they are also involved in regulation of other biological functions, including sleep and metabolism.



